The Importance of Self-Monitoring in Type 2 Diabetes
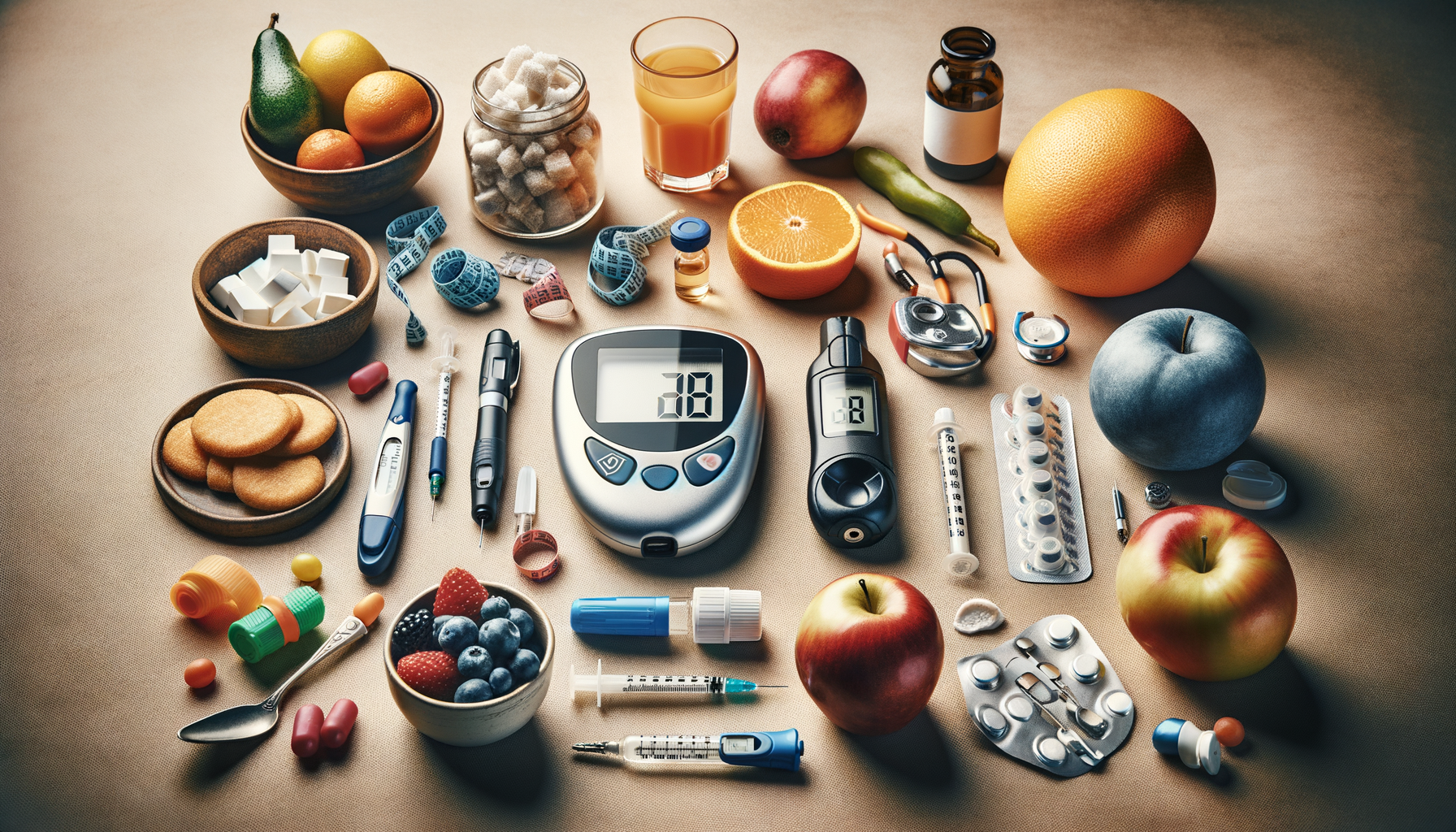
Self-monitoring of blood glucose (SMBG) is a cornerstone in the management of type 2 diabetes. It provides real-time feedback on how food, physical activity, and medications affect blood sugar levels. This data is crucial for making informed decisions about diet and lifestyle changes. Research shows that consistent self-monitoring can lead to improved glycemic control, reducing the risk of complications such as neuropathy and cardiovascular diseases.
One of the key benefits of SMBG is the ability to detect patterns and trends in blood sugar levels. By keeping a detailed log, individuals can identify which foods cause spikes or dips in glucose levels, allowing for better dietary choices. Moreover, it allows healthcare providers to tailor treatment plans more effectively. For instance, if a patient frequently experiences high blood sugar in the morning, adjustments in medication or dietary recommendations can be made.
However, self-monitoring is not just about numbers. It’s about understanding what those numbers mean and how to respond. For many, this involves learning to recognize the signs of hyperglycemia and hypoglycemia and knowing how to manage these situations. Regular monitoring also fosters a sense of responsibility and empowerment, encouraging proactive management of the condition.
Effective Treatment Strategies for Type 2 Diabetes
Managing type 2 diabetes effectively requires a multi-faceted approach. While medication plays a crucial role, lifestyle modifications are equally important. A balanced diet, regular physical activity, and weight management are vital components of a successful treatment plan.
Dietary changes should focus on reducing simple carbohydrates and sugars, while increasing fiber intake. Foods rich in whole grains, vegetables, and lean proteins are recommended. These choices help stabilize blood sugar levels and promote overall health. Additionally, portion control and meal timing can significantly impact glucose management.
Physical activity is another critical element. Regular exercise helps increase insulin sensitivity and lowers blood sugar levels. Activities such as walking, swimming, or cycling are beneficial and can be tailored to individual fitness levels. The goal is to incorporate at least 150 minutes of moderate exercise per week.
Medications, including oral hypoglycemics and insulin, are often necessary to achieve optimal blood sugar control. It’s essential to follow the prescribed regimen and communicate with healthcare providers about any side effects or concerns. Regular check-ups and blood tests are necessary to monitor progress and make necessary adjustments to the treatment plan.
The Role of Technology in Diabetes Management
Technology has revolutionized diabetes management, offering tools that simplify tracking and monitoring. Devices such as continuous glucose monitors (CGMs) provide real-time data and alerts, helping users maintain target glucose levels. These devices reduce the need for frequent finger-pricking, making glucose monitoring less intrusive and more convenient.
Smartphone apps also play a significant role. They offer features such as food logging, exercise tracking, and medication reminders. Many apps integrate with CGMs, providing a comprehensive view of a user’s health data. This integration allows for more precise adjustments to diet and medication, tailored to individual needs.
Telemedicine has emerged as a vital resource, especially for those with limited access to healthcare facilities. Virtual consultations enable patients to discuss their condition with healthcare providers, receive advice, and adjust treatment plans without leaving home. This accessibility is crucial for maintaining consistent care and support.
While technology offers numerous benefits, it’s important to select tools that are user-friendly and meet individual needs. Not all devices and apps are suitable for everyone, and personal preferences should guide the choice of technology. It’s also essential to ensure data privacy and security when using digital health tools.
Common Challenges and How to Overcome Them
Managing type 2 diabetes can be challenging, with many individuals facing obstacles that hinder effective self-care. One common issue is the feeling of being overwhelmed by the need for constant monitoring and lifestyle changes. To combat this, setting realistic goals and celebrating small achievements can provide motivation and a sense of accomplishment.
Another challenge is maintaining a healthy diet, especially when dining out or during social gatherings. Planning ahead and making informed choices can help navigate these situations. It’s also beneficial to communicate dietary needs to hosts or restaurant staff to ensure suitable options are available.
Adherence to medication regimens can be difficult, particularly if side effects occur. Open communication with healthcare providers is essential to address these concerns and explore alternative treatments if necessary. Support groups and counseling can also offer encouragement and practical advice from others experiencing similar challenges.
Financial constraints may pose a barrier to accessing medications, technology, or healthcare services. Exploring insurance options, seeking assistance programs, and discussing cost-effective alternatives with healthcare providers can alleviate some of these burdens.
Building a Support System for Long-Term Success
Having a strong support system is invaluable in managing type 2 diabetes. Family, friends, and healthcare professionals can provide encouragement, accountability, and practical assistance. Involving loved ones in the management plan can foster understanding and cooperation, making lifestyle changes more manageable.
Support groups, whether in-person or online, offer a platform for sharing experiences, advice, and emotional support. Connecting with others who face similar challenges can reduce feelings of isolation and provide fresh perspectives on problem-solving.
Healthcare providers are a critical part of the support network. Regular consultations with doctors, dietitians, and diabetes educators ensure that treatment plans remain effective and up-to-date. These professionals can offer guidance on managing complications and adjusting strategies as needed.
Ultimately, building a support system involves open communication, mutual respect, and a willingness to seek help when needed. By fostering a collaborative environment, individuals with type 2 diabetes can achieve better health outcomes and enjoy a higher quality of life.