Understanding Psoriasis: A Brief Overview
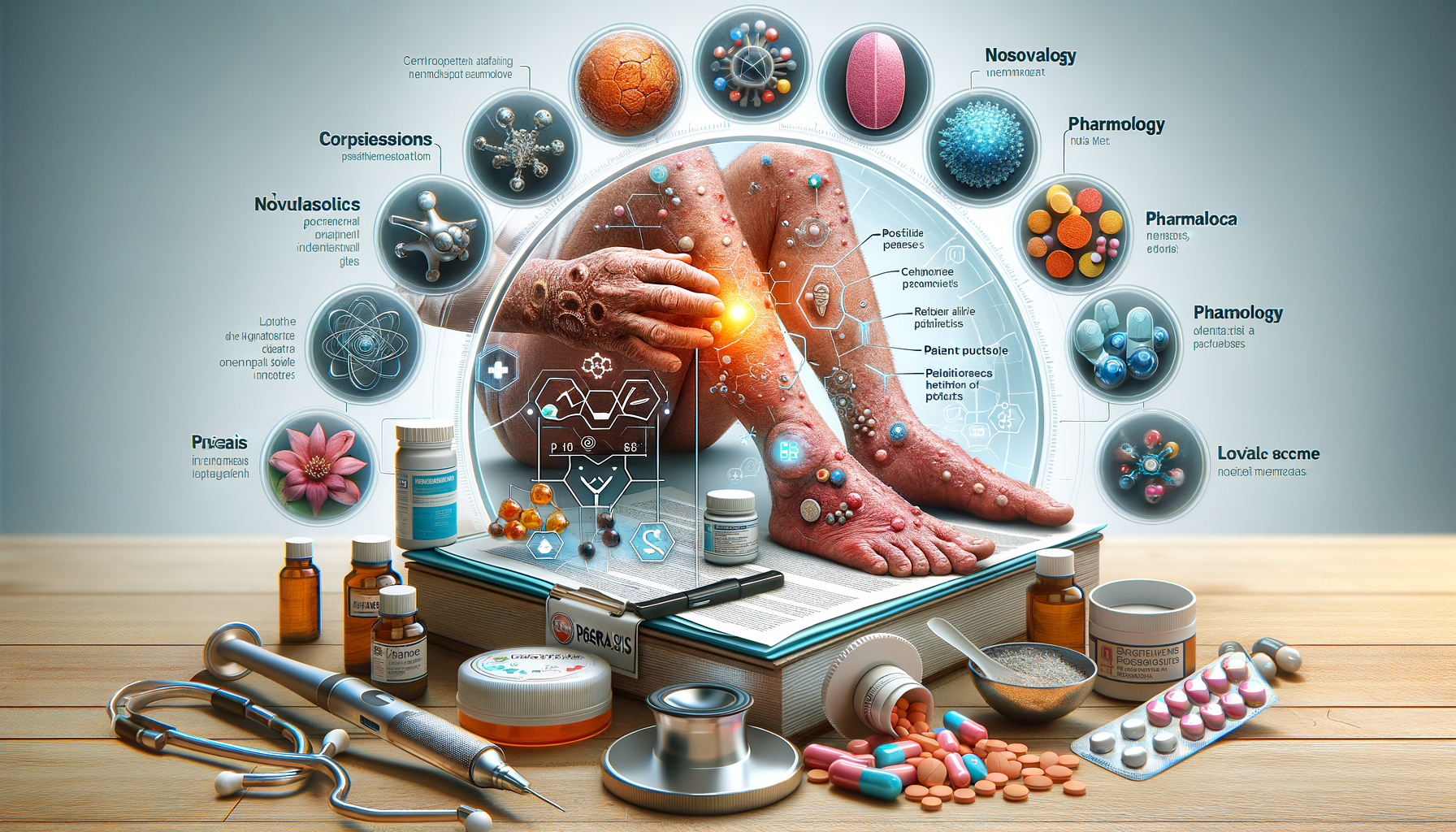
Psoriasis is a chronic autoimmune condition that causes rapid skin cell production, leading to scaling on the skin’s surface. This disease affects over 125 million people worldwide, highlighting its global prevalence and the need for effective management strategies. The symptoms of psoriasis vary, but they often include red patches of skin covered with thick, silvery scales, dry and cracked skin that may bleed, and itching or burning sensations. The psychological impact of psoriasis cannot be understated, as many individuals experience significant emotional distress, impacting their quality of life.
Understanding the nature of psoriasis is crucial for both patients and healthcare providers. The condition is not merely a skin disorder; it is a systemic issue that can be associated with other health problems such as psoriatic arthritis, cardiovascular diseases, and depression. This multifaceted nature of psoriasis necessitates a comprehensive approach to treatment that addresses both the physical and psychological aspects of the disease.
Traditional Treatment Options
Traditional treatments for psoriasis have focused on managing symptoms and slowing the progression of the disease. Topical treatments, such as corticosteroids and vitamin D analogues, are commonly prescribed as first-line treatments. These medications aim to reduce inflammation and slow down the excessive production of skin cells. Despite their effectiveness, these treatments often require continuous application and may cause side effects, such as skin thinning or irritation.
Phototherapy, another traditional treatment, involves exposing the skin to ultraviolet light under medical supervision. This method can be effective, particularly for individuals with moderate to severe psoriasis. However, the need for frequent clinic visits and potential long-term risks, such as skin cancer, can be limiting factors.
Systemic treatments, including oral medications and injections, are often reserved for severe cases. These treatments work throughout the body and can be effective in reducing symptoms. However, they may come with significant side effects, such as liver damage or increased risk of infection, necessitating careful monitoring by healthcare professionals.
Innovative Treatments: Biologics and Beyond
In recent years, biologic drugs have emerged as a groundbreaking treatment option for psoriasis. These medications target specific parts of the immune system, offering a more precise approach to treatment. Biologics are often used for moderate to severe psoriasis when traditional treatments are ineffective. They can significantly reduce symptoms and improve quality of life for many patients. However, they require administration through injections or infusions, which can be a barrier for some individuals.
Another innovative treatment is the use of small molecule inhibitors, which target specific enzymes within the immune system. These oral medications offer an alternative to biologics and have shown promise in clinical trials. The development of these treatments reflects a broader trend in psoriasis management towards personalized medicine, where therapies are tailored to individual patient needs and genetic profiles.
Despite their potential, innovative treatments can be costly and may not be accessible to all patients. Insurance coverage and healthcare policies play a significant role in determining the availability of these treatments. Ongoing research and advocacy are essential to expanding access and ensuring that all individuals with psoriasis can benefit from the latest advancements in care.
Lifestyle and Home Remedies
While medical treatments are essential for managing psoriasis, lifestyle changes and home remedies can play a supportive role in alleviating symptoms. Maintaining a healthy lifestyle can help reduce flare-ups and improve overall well-being. Here are some strategies that can complement medical treatment:
- Diet: A balanced diet rich in fruits, vegetables, lean proteins, and healthy fats can support immune function and reduce inflammation.
- Stress Management: Techniques such as meditation, yoga, and deep breathing can help reduce stress, which is known to trigger psoriasis flare-ups.
- Moisturizing: Regularly applying moisturizers can prevent dryness and reduce scaling. Opt for fragrance-free products to minimize irritation.
- Avoiding Triggers: Identifying and avoiding personal triggers, such as certain foods or environmental factors, can help manage symptoms.
It’s important to note that while these lifestyle changes can support treatment, they are not a substitute for medical care. Patients should work closely with their healthcare providers to develop a comprehensive treatment plan that includes both medical and lifestyle approaches.
Support Systems and Resources
Living with psoriasis can be challenging, but support systems and resources are available to help individuals manage the condition effectively. Patient support groups, both online and in-person, offer a platform for sharing experiences, advice, and emotional support. These communities can be invaluable for individuals feeling isolated or overwhelmed by their condition.
Healthcare providers play a critical role in offering guidance and support. Regular check-ins with dermatologists and other specialists ensure that treatment plans are effective and adjusted as needed. Additionally, mental health professionals can provide support for managing the psychological impact of psoriasis, such as anxiety and depression.
Educational resources, such as websites and literature from reputable health organizations, offer information on the latest research and treatment options. These resources empower patients to make informed decisions about their health and advocate for their needs within the healthcare system.
Ultimately, a strong support network and access to reliable information are crucial components of effective psoriasis management. By leveraging these resources, individuals with psoriasis can navigate their condition with confidence and improve their quality of life.
Conclusion: Empowering Individuals with Psoriasis
Psoriasis is a complex and multifaceted condition that requires a comprehensive approach to treatment. By understanding the various treatment options available, from traditional methods to innovative therapies, individuals can make informed decisions about their care. Lifestyle changes and support systems further enhance treatment outcomes, providing a holistic approach to managing the disease.
Empowering individuals with knowledge and resources is key to improving quality of life for those living with psoriasis. With ongoing research and advancements in treatment, there is hope for more effective and accessible solutions in the future. By working together with healthcare providers and support networks, individuals with psoriasis can navigate their journey with resilience and optimism.